Regular IVF (with ICSI & AZH)
Overview
Regular In vitro fertilization (IVF) with ICSI & AZH is a complicated set of techniques designed to improve fertility, avoid genetic abnormalities, and aid in childbirth.
During IVF, mature eggs are extracted from the ovaries and fertilized in a laboratory using sperm. The fertilized egg (embryo) or eggs (embryos) are then placed in the uterus. A whole IVF cycle takes roughly three weeks. When these processes are divided into sections, the procedure might take longer.
The most effective kind of assisted reproductive technology is IVF with ICSI or AZH. The treatment can be performed with the couple's own eggs and sperm. Alternatively, IVF may use eggs, sperm, or embryos from a known or anonymous donor. A gestational carrier, or someone who has an embryo implanted in their uterus, may be employed in some instances.
Many variables influence your odds of having a healthy baby with IVF, including your age and the cause of infertility. Furthermore, IVF can be time-consuming, expensive, and invasive. IVF can result in a pregnancy with more than one fetus if more than one embryo is implanted to the uterus (multiple pregnancy).
Your doctor can help you understand how IVF works, the potential risks and whether this method of treating infertility is right for you.
What is Intracytoplasmic Sperm Injection (ICSI)?
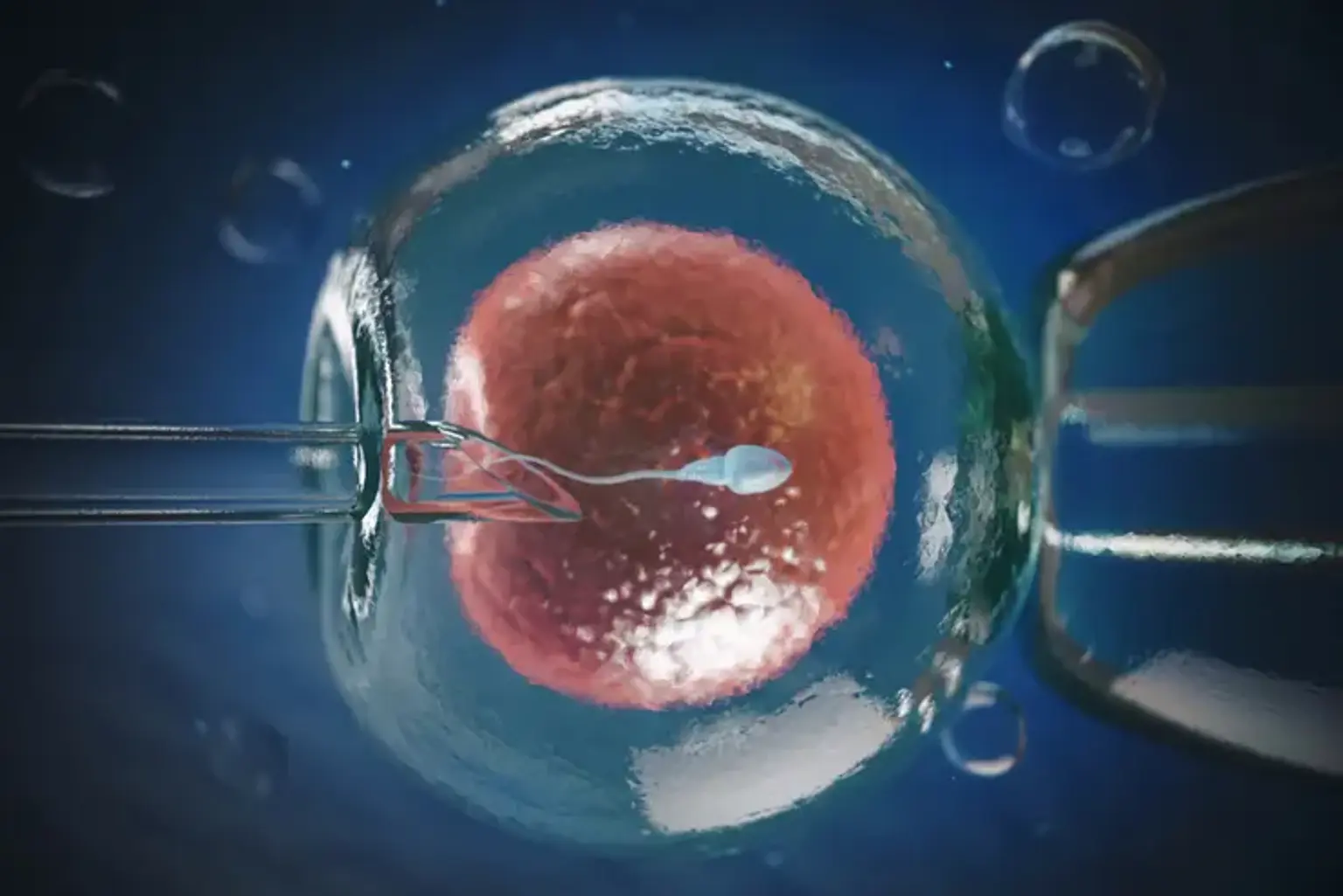
Intracytoplasmic sperm injection (ICSI) is a laboratory process in which a single sperm is injected directly into the cytoplasm of a mature egg via micromanipulation. When there are anomalies in the amount, quality, or function of the sperm, or when there are issues with sperm entry of the egg, this procedure raises the chance of conception. ICSI must be performed concurrently with an in-vitro fertilization cycle.
Who Benefits From ICSI?
- Couples who have been diagnosed with infertility owing to male factor infertility. Male factor infertility can be caused by a number of diseases. Sperm might be totally missing in the ejaculate, which is known as azoospermia, or males can have extremely low sperm densities in the ejaculate, which is known as oligospermia. Poor sperm motility, also known as asthenospermia, occurs when the sperm lacks the forward swimming motion required to join with the egg in the female oviduct. Men who are infertile may also have teratospermia, which is a higher percentage of improperly shaped sperm. There may also be issues with sperm function, reducing their capacity to bind and/or fertilize the egg.
- Patients who had previously failed natural conception during an IVF round. Even if the male partner appears to have normal sperm counts, motility, and morphology, this can happen.
- Patients who use frozen sperm, which may be restricted in quantity and/or quality.
- Antisperm antibodies linked to spermatozoa or female antisperm antibodies are suspected of causing infertility.
- Patients with a limited quantity of eggs who desire to increase their chances of fertilization.
What is Assisted Zona Hatching (AZH)?
In some cases, assisted zona hatching (AZH) may enhance the chances of embryo implantation and pregnancy. The zona pellucida is a "shell" that protects the preimplantation embryo. This shell is necessary for embryo development up to the blastocyst stage (about day 5). Once the blastocyst has formed, the embryo must break free from the zona pellucida (hatch) in order to implant and become pregnant.
AZH is a micromanipulation procedure utilized on Day 3 of embryo development. Embryos are typically 6 to 8 cells in size. A laser is used to create a hole in the embryo's zona during the AZH therapy. This is done a few hours before the embryo transfer.
When the embryo matures as a blastocyst in the uterus, this break in the zona pellucida allows it to hatch free of the zona pellucida. One possible cause for implantation failure is that the embryo is unable to leave the zona pellucida.
Who Benefits From AZH?
Assisted hatching is most useful for the following types of patients:
- Patients who are older than 38 years of age.
- Patients with elevated levels of follicle stimulating hormone (FSH).
- Patients whose embryos have a thicker than normal zona pellucida, as measured by trained embryologists.
- Patients who have had multiple previous IVF attempts with failed implantation.
In Vitro Fertilization (IVF)
In vitro fertilization (IVF) is a method of treating infertility or genetic disorders. If IVF is used to treat infertility, you and your spouse may be able to try less intrusive treatment options first, such as fertility medicines to enhance egg production or intrauterine insemination – a process in which sperm are inserted directly in the uterus near the time of ovulation.
IVF is sometimes recommended as a main therapy for infertility in women over the age of 40. If you have specific medical issues, IVF can also be performed. For example, if you or your partner suffers from:
- Fallopian tube damage or blockage. Fallopian tube damage or blockage makes it difficult for an egg to be fertilized or for an embryo to travel to the uterus.
- Ovulation disorders. If ovulation is infrequent or absent, fewer eggs are available for fertilization.
- Endometriosis. Endometriosis occurs when tissue similar to the lining of the uterus implants and grows outside of the uterus — often affecting the function of the ovaries, uterus and fallopian tubes.
- Uterine fibroids. Fibroids are benign tumors in the uterus. They are common in women in their 30s and 40s. Fibroids can interfere with implantation of the fertilized egg.
- Previous tubal sterilization or removal. Tubal ligation is a method of sterilization that involves cutting or blocking the fallopian tubes to permanently prevent conception. If you want to get pregnant after tubal ligation, IVF may be a better option than tubal ligation reversal surgery.
- Impaired sperm production or function. Poor sperm motility, low sperm concentration, or abnormalities in sperm size and shape might make it difficult for sperm to fertilize an egg. If abnormalities in the sperm are discovered, a visit to an infertility expert may be required to determine whether there are any correctable issues or underlying health concerns.
- Unexplained infertility. Unexplained infertility means no cause of infertility has been found despite evaluation for common causes.
- A genetic disorder. If you or your spouse are at risk of passing on a genetic condition to your kid, you may be a candidate for IVF-based preimplantation genetic testing. After the eggs have been retrieved and fertilized, they are checked for genetic issues, although not all genetic disorders may be detected. Embryos that do not have any known abnormalities can be transplanted to the uterus.
- Fertility preservation for cancer or other health conditions. If you are going to begin cancer treatment that may affect your fertility, such as radiation or chemotherapy, IVF for fertility preservation may be a possibility. Women can have their eggs removed from their ovaries and frozen unfertilized for future use. Alternatively, the eggs might be fertilized and saved as embryos for later use. Women who do not have a functioning uterus or for whom pregnancy offers a significant health risk may choose for IVF with another person carrying the fetus (gestational carrier). The woman's eggs are fertilized with sperm in this situation, but the resultant embryos are implanted in the gestational carrier's uterus.
Risks oF Regular IVF With AZH/ICSI
Risks include:
- Multiple births. IVFwith AZH/ICSI increases the risk of multiple births if more than one embryo is transferred to your uterus. A pregnancy with multiple fetuses carries a higher risk of early labor and low birth weight than pregnancy with a single fetus does.
- Premature delivery and low birth weight. Research suggests that IVF slightly increases the risk that the baby will be born early or with a low birth weight.
- Ovarian hyperstimulation syndrome. Use of injectable fertility drugs, such as human chorionic gonadotropin (HCG), to induce ovulation can cause ovarian hyperstimulation syndrome, in which your ovaries become swollen and painful.
Symptoms typically last a week and include mild abdominal pain, bloating, nausea, vomiting and diarrhea. If you become pregnant, however, your symptoms might last several weeks. Rarely, it's possible to develop a more severe form of ovarian hyperstimulation syndrome that can also cause rapid weight gain and shortness of breath.
- Miscarriage. The rate of miscarriage for women who conceive using IVF with fresh embryos is similar to that of women who conceive naturally — about 15% to 25% — but the rate increases with maternal age.
- Egg-retrieval procedure complications. Use of an aspirating needle to collect eggs could possibly cause bleeding, infection or damage to the bowel, bladder or a blood vessel. Risks are also associated with sedation and general anesthesia, if used.
- Ectopic pregnancy. About 2% to 5% of women who use IVF will have an ectopic pregnancy — when the fertilized egg implants outside the uterus, usually in a fallopian tube. The fertilized egg can't survive outside the uterus, and there's no way to continue the pregnancy.
- Birth defects. The age of the mother is the primary risk factor in the development of birth defects, no matter how the child is conceived. More research is needed to determine whether babies conceived using IVF might be at increased risk of certain birth defects.
- Cancer. Although early research revealed a relationship between some drugs used to increase egg formation and the development of a certain kind of ovarian tumor, more current research contradicts these findings. Following IVF, there does not appear to be a significantly increased risk of breast, endometrial, cervical, or ovarian cancer.
- Stress. Use of IVF can be financially, physically and emotionally draining. Support from counselors, family and friends can help you and your partner through the ups and downs of infertility treatment.
How You Prepare?
Individual pregnancy and live birth rates at U.S. clinics are available online from the Centers for Disease Control and Prevention and the Society for Assisted Reproductive Technology.
The success rate of a clinic is determined by a variety of factors. These include the ages and medical conditions of the patients, as well as the clinic's treatment population and treatment procedures. Ask about the charges involved with each phase of the operation in detail.
Before beginning a cycle of IVF using your own eggs and sperm, you and your partner will likely need various screenings, including:
- Ovarian reserve testing. Your doctor may test the concentrations of follicle-stimulating hormone (FSH), estradiol (estrogen), and anti-mullerian hormone in your blood during the first few days of your menstrual cycle to evaluate the amount and quality of your eggs. The findings of the tests, which are frequently combined with an ultrasound of your ovaries, can help anticipate how your ovaries will respond to reproductive medicine.
- Semen analysis. If not done as part of your initial fertility evaluation, your doctor will conduct a semen analysis shortly before the start of an IVF treatment cycle.
- Infectious disease screening. You and your partner will both be screened for infectious diseases, including HIV.
- Practice (mock) embryo transfer. Your doctor might conduct a mock embryo transfer to determine the depth of your uterine cavity and the technique most likely to successfully place the embryos into your uterus.
- Uterine exam. Before you begin IVF, your doctor will inspect the uterine lining. A sonohysterogram (in which fluid is injected through the cervix into your uterus) and an ultrasound to produce pictures of your uterine cavity may be used. It might also entail a hysteroscopy, which involves inserting a thin, flexible, lighted telescope (hysteroscope) through your vagina and cervix into your uterus.
Steps of the Procedure
IVF can be broken down into the following steps:
Birth control pills or estrogen:
Your doctor may prescribe birth control pills or estrogen before you begin IVF therapy. This is used to prevent the formation of ovarian cysts and to regulate the time of your menstrual cycle. It enables your doctor to manage your therapy and optimize the number of mature eggs obtained during the egg retrieval operation. Some people are given estrogen and progesterone combination birth control tablets, while others are given only estrogen.
Ovarian stimulation:
Each month, a set of eggs begins to grow throughout the natural cycle of a healthy person of reproductive age. Typically, only one egg matures to the point of ovulation. That group's remaining immature eggs disintegrate.
During your IVF round, you'll be given injectable hormone drugs to encourage the whole batch of eggs in that cycle to mature at the same time and completely. This means that instead of having one egg (as in a natural cycle), you might have numerous eggs. Based on your medical history, age, AMH (anti-mullerian hormone) level, and response to ovarian stimulation during previous IVF cycles, the kind, dose, and frequency of drugs administered will be personalized to you as an individual.
Egg retrieval:
- Your healthcare provider uses an ultrasound to guide a thin needle into each of your ovaries through your vagina. The needle is connected to a suction device used to pull your eggs out of each follicle.
- Your eggs are placed in a dish containing a special solution. The dish is then put in an incubator (controlled environment).
- Medication and mild sedation are used to reduce discomfort during this procedure.
- Egg retrieval is done 36 hours after your last hormone injection, the “trigger shot.”
Fertilization:
The embryologist will attempt to fertilize all mature eggs using intracytoplasmic sperm injection, or ICSI, the afternoon after your egg retrieval operation. This implies that each developed egg will be injected with sperm. ICSI cannot be conducted on immature eggs. The immature eggs will be put in a dish that also contains sperm and nutrition. Immature eggs seldom complete their development in the dish. If an immature egg matures, the sperm in the dish might try to fertilize it.
70% of mature eggs will fertilize on average. For example, if ten ripe eggs are collected, about seven will fertilize. If the fertilization is successful, the fertilized egg will develop into an embryo.
If there are an exceedingly large number of eggs or you don’t want all eggs fertilized, some eggs may be frozen before fertilization for future use.
Embryo development:
Your embryos' development will be closely watched over the following five to six days.
Your embryo must overcome substantial obstacles before it can be transferred to your uterus. 50% of fertilized embryos reach the blastocyst stage on average. This is the best time to transfer to your uterus. For instance, if seven eggs are fertilized, three or four may develop to the blastocyst stage. The remaining 50% usually do not advance and are discarded.
On day five or six after fertilization, any embryos eligible for transfer will be preserved and used for future embryo transfers.
Embryo transfer:
Fresh embryo transfer and frozen embryo transfer are the two types of embryo transfers. Your healthcare professional can help you decide whether to use fresh or frozen embryos based on your specific scenario. The identical transfer procedure is used for frozen and fresh embryo transfers. The name implies the primary distinction.
A fresh embryo transfer involves inserting your embryo into your uterus between three and seven days following the egg retrieval operation. This embryo has not been frozen and is hence "fresh."
Frozen embryos (from a previous IVF cycle or donor eggs) are thawed and put into your uterus during a frozen embryo transfer. This is a more usual treatment for logistical reasons and because it results in a more probable live delivery. Transferring frozen embryos can happen years after egg extraction and fertilization.
To prepare your uterus for absorbing an embryo, you'll take oral, injectable, vaginal, or transdermal hormones as part of the initial stage of a frozen embryo transfer. This is usually followed by 14 to 21 days of oral medicine and six days of injections. During this period, you'll often have two or three sessions to assess the readiness of your uterus with ultrasound and to measure your hormone levels with a blood test. When your uterus is ready, the embryo transfer operation will be planned for you. When utilizing fresh embryos, the procedure is similar, except that embryo transfer occurs within three to five days following retrieval.
The embryo transfer process is easy and does not require anesthesia. It feels like a pelvic exam or a Pap smear. A speculum is placed within the vagina, and a thin catheter is inserted through the cervix into the uterus. A syringe attached to the other end of the catheter contains one or more embryos. The embryos are injected it the uterus through the catheter. The procedure typically takes less than 10 minutes.
Pregnancy:
Pregnancy begins when the embryo implants itself into the uterine lining. Approximately nine to 14 days following embryo transfer, your healthcare professional will conduct a blood test to determine if you are pregnant.
The same procedures are followed if donor eggs are utilized. Ovarian stimulation and egg retrieval will be completed by the egg donor. Following fertilization, the embryo is delivered to the person who will carry the pregnancy (either with or without various fertility medications).
There are several considerations to consider before beginning IVF therapy. It is critical to contact with your healthcare physician to have a thorough understanding of the IVF procedure and what to expect.
Results & Outcome
About 12 days to two weeks after egg retrieval, your doctor will test a sample of your blood to detect whether you're pregnant.
- If you're pregnant, your doctor will refer you to an obstetrician or other pregnancy specialist for prenatal care.
- If you're not pregnant, you'll stop taking progesterone and likely get your period within a week. If you don't get your period or you have unusual bleeding, contact your doctor. If you're interested in attempting another cycle of in vitro fertilization (IVF), your doctor might suggest steps you can take to improve your chances of getting pregnant through IVF.
The chances of giving birth to a healthy baby after using IVF depend on various factors, including:
- Maternal age. The younger you are, the more likely you are to get pregnant and give birth to a healthy baby using your own eggs during IVF. Women age 41 and older are often counseled to consider using donor eggs during IVF to increase the chances of success.
- Embryo status. Transfer of embryos that are more developed is associated with higher pregnancy rates compared with less-developed embryos (day two or three). However, not all embryos survive the development process. Talk with your doctor or other care provider about your specific situation.
- Reproductive history. Women who've previously given birth are more likely to be able to get pregnant using IVF than are women who've never given birth. Success rates are lower for women who've previously used IVF multiple times but didn't get pregnant.
- Cause of infertility. Having a normal supply of eggs increases your chances of being able to get pregnant using IVF. Women who have severe endometriosis are less likely to be able to get pregnant using IVF than are women who have unexplained infertility.
- Lifestyle factors. Women who smoke typically have fewer eggs retrieved during IVF and may miscarry more often. Smoking can lower a woman's chance of success using IVF by 50%. Obesity can decrease your chances of getting pregnant and having a baby. Use of alcohol, recreational drugs, excessive caffeine and certain medications also can be harmful.
Conclusion
Infertility is a prevalent medical disease that affects a big number of couples throughout the world. Several infertility therapies are now accessible as a result of modern medical breakthroughs. These terms are frequently used to refer to in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI), a specialized form of IVF. IVF and ICSI are becoming increasingly popular because to their excellent success rates.
However, the most often asked questions are if these treatments can provide a 100 percent probability of pregnancy the first time and whether the created embryo will be fully developed to produce a healthy kid. The methods of assisted fertilization techniques change in order to boost the chances of conception. It is critical to grasp the fundamentals of the ovulation and fertilization processes, as well as pregnancy and delivery.
The most appropriate technique for each couple will be discussed by the fertility specialist based on particular couple’s conditions and relevant infertile problems.